Training Guide
| HMO | stands for Health Maintenance Organization is a healthcare delivery system that most employees are entitled to use as part of the benefit they receive from their employers. |
| TPA | stands for Third Party Administrator and as such is defined as an organization or individual that handles the claims, processing, and reporting components of a self-funded health benefits plan. |
| MBL | stands for maximum benefit limit refers to the consumable limit one can use per treatment/illnesses, per person, per year. |
| ABL | stands for annual benefit limit refers to the maximum aggregate limit in availing applicable benefits and services limited to covered illnesses on a per member per year or per family unit per year basis as may be applicable. |
| INNER LIMIT | refers to a specific cap or limit on certain types of coverage, often within a broader or more general policy limit. Essentially, the "inner limit" is a sub-limit or a restrained cap placed on specific medical treatments, procedures, or services, even if the overall coverage limit (the total sum the insurer will pay) is higher. |
| UTILIZATION | refers to the use or consumption of healthcare services by policyholders or beneficiaries. It essentially measures how often and to what extent people are utilizing the benefits and services provided under their health insurance plan. |
| EXCLUSION or UNCOVERED ITEMS |
refers to specific conditions, treatments, or situations that are not covered by an insurance policy. These are exceptions where the insurer will not provide financial coverage or reimburse costs, even if the condition or treatment is medically necessary. Exclusions are typically listed in the policy document and are an important part of the terms and conditions of the insurance contract. |
| PRE-EXISTING CONDITION (PEC) | stands for preexisting condition is a term that refers to a known illness, injury, or health condition that existed before someone enrolls in or begins receiving health or life insurance. |
| DREADED CONDITIONS | This corresponds to any condition that is considered to be chronic, progressive, life-threatening and which may entail lifelong therapy |
| ACCREDITED | (of a person, organization, or course of study) officially recognized or authorized. |
| NON-ACCREDITED | not recognized as meeting prescribed standards or requirements |
| UMBRELLA ACCREDITATION | refers to the process where a health insurance company recognizes the accreditation of a hospital system or healthcare network as a whole, rather than accrediting each individual hospital or facility within that network separately. |
| NON-UMBRELLA ACCREDITATION | refers to a situation where each individual hospital or healthcare facility within a hospital network is separately accredited by a recognized accrediting body, rather than having a blanket accreditation for the entire system (as in umbrella accreditation). In this case, the health insurance company must evaluate and verify the accreditation status of each hospital or facility independently, to ensure they meet the insurer's standards for inclusion in their provider network. |
| PROVIDER | healthcare providers - clinic and hospitals. |
| LOA | stands for Letter of Authorization is a letter that authorizes an Amaphil member to avail their needed medical availment in the accredited healthcare partner of Amaphil. |
| SOB | stands for Schedule Of Benefits is a list of the various services covered under a health insurance plan |
| ICD CODE | stands for International Classification of Diseases codes are a set of designations used by healthcare staff to communicate diseases, symptoms, abnormal findings, and other elements of a patient's diagnosis in a way that is universally accepted by those in the medical and insurance fields. |
| CPT CODE | stands for Current Procedural Terminology (CPT®) codes offer doctors and health care professionals a uniform language for coding medical services and procedures to streamline reporting, increase accuracy and efficiency. |
| RUV CODE | stands for Relative Value Unit a number assigned to compensable services provided by a physician. |
| RVS CODE | stands for relative value scale is a key element in the construction of a physician fee |
Telephone etiquette refers to the set of polite behaviors and best practices used when communicating over the phone. It's important for maintaining professionalism and ensuring smooth, respectful interactions. Here are key guidelines for proper telephone etiquette:
1. Answering the Phone
- Be prompt: Answer the phone within a few rings. Ideally, within three to four rings.
- Greet the caller: Start with a friendly greeting, such as "Good morning" or "Hello." If you are answering a business call, include your name and the company or department you represent, for example, "Hello, this is [Your Name] from [Company]. How can I help you?"
- Be polite: Use phrases like "Please" and "Thank you" during the conversation.
2. During the Call
- Listen actively: Pay close attention to the caller and avoid interrupting them. If necessary, take notes for clarity.
- Speak clearly: Ensure your voice is clear and at an appropriate volume. Speak slowly enough to be understood, but not too slowly.
- Be concise: Get to the point without unnecessary rambling, especially in business or professional calls.
- Stay positive and calm: Even if the conversation becomes difficult, try to maintain a positive and professional tone. Avoid sounding frustrated or rude.
3. Handling Hold and Transfers
- Ask permission: If you need to place someone on hold, always ask first, saying something like "May I place you on hold for a moment?" Wait for their approval before doing so.
- Provide updates: If the wait is going to be longer than expected, periodically check back with the caller to update them.
- Transfer politely: When transferring a call, explain the reason and give the caller the name of the person they will be speaking to, for example, "I’ll transfer you to [Name], who can help you with that."
4. Making the Call
- Introduce yourself: When initiating a call, introduce yourself first and explain the purpose of the call.
- Be mindful of timing: Call during appropriate hours. Avoid calling early in the morning, late in the evening, or during lunch hours unless it's urgent.
- Prepare for the conversation: Before making a call, gather any necessary information and know what you want to discuss to avoid wasting time.
5. Ending the Call
- Summarize the conversation: Before hanging up, briefly summarize any key points or actions that need to be taken.
- Thank the caller: Always thank the person for their time. A simple "Thank you for calling" or "I appreciate your time" is courteous.
- Say goodbye politely: End the conversation with a polite "Goodbye" or "Have a great day," and wait for the other person to hang up first.
7. General Tips
- Avoid distractions: Try to avoid distractions during a call, such as eating, typing, or background noise.
- Respect privacy: Avoid discussing personal or sensitive matters in public or shared spaces, especially during business calls.
- Mind your tone: Since tone and body language aren't visible over the phone, make sure your voice conveys the right message. A warm tone is more inviting than a monotone or harsh tone.
Good telephone etiquette helps in building rapport, fostering trust, and ensuring effective communication. Whether in personal or professional settings, practicing these guidelines will lead to more positive and productive conversations.
OUTPATIENT BASIC CONSULTATION and OUTPATIENT-REFERRAL-TO-SPECIALIST
Medical consultation refers to a meeting or interaction between a patient and a healthcare provider (typically a doctor, specialist, or other medical professional) in order to evaluate, diagnose, and provide treatment recommendations for the patient’s health concerns. It is a key component of the healthcare process and can take place in various settings such as a clinic, hospital, or through telemedicine.
OUTPATIENT CLINIC-SETTING and OUTPATIENT-LABORATORY
Clinic-setting procedures are minor medical procedures may be performed directly in the clinic. These procedures often involve basic or non-invasive treatments.
Laboratory tests are a critical part of the diagnostic process in healthcare. These tests help healthcare providers assess a patient’s health, diagnose conditions, monitor ongoing treatments, and detect diseases early. They are often used to measure various substances in a patient’s blood, urine, or other bodily fluids to gain insights into the function of organs and overall health status.
Imaging tests are medical procedures that use various technologies to create visual representations of the interior of the body. These tests are crucial for diagnosing, monitoring, and guiding treatment for various medical conditions. They help healthcare providers see structures inside the body, detect abnormalities, and assess the progress of diseases. Imaging tests are non-invasive (except for some specific types) and provide a clear view of tissues, bones, organs, and vessels, assisting in precise diagnosis and treatment planning.
EMERGENCY (ER)
Emergency care typically falls under a category called "Emergency Medical Services" or "Emergency Care" availment. This refers to immediate medical attention for severe or life-threatening conditions that require prompt treatment to prevent serious harm, disability, or death.
OUT-PATIENT SURGERY (OPD-OR)
The term "OP or" in a medical context typically refers to "Outpatient Operating Room" or "Outpatient Surgery". It is used in settings where surgeries or procedures are performed on patients who do not require an overnight stay in the hospital. The patient comes in for the procedure and leaves the same day.
IN-PATIENT ADMISSION AND DISCHARGE
Inpatient admission refers to the process of a patient being formally admitted to a hospital or medical facility for treatment, where they are required to stay overnight or for a longer duration. This type of admission is necessary when a patient requires intensive care, monitoring, or a surgical procedure that needs more than just a brief visit or outpatient care.
Inpatient discharge refers to the process in which a patient is formally released from the hospital after being admitted for care. It occurs when the patient no longer requires inpatient care, has recovered sufficiently, or is stable enough to continue recovery at home or in a less intensive care setting (such as a rehabilitation facility or long-term care facility). The discharge process involves several steps to ensure that the patient’s medical, emotional, and logistical needs are met for the next phase of recovery.
Procedure
Is the LOA issued to the correct member? (tracker vs LOA)
Is it issued to the correct facility? (tracker vs LOA)
Does the patient have access to the facility? (Major hospital/Alster CTS-clinic only for OP)
Is the availment tagged correctly?
Are the diagnoses covered based on the benefit of the patient? (check exclusion/inner limit)
Are the procedures covered based on the benefit of the patient? (check exclusion/inner limit)
Are the procedures related to the diagnoses?
Is the LOA amount within the benefit coverage of the patient? (Plan vs Util)
Consultation
Is the LOA issued to the correct member? (tracker vs LOA)
Is it issued to the correct facility? (tracker vs LOA)
Does the patient have access to the facility? (Major hospital/Alster CTS-clinic only for OP)
Is the availment tagged correctly?
Is the chief complaint covered?
Is the LOA amount within the benefit coverage of the patient? (Plan vs Util)
UNLESS EXCEPTIONS TO THE FOLLOWING GENERAL EXCLUSIONS ARE MADE UNDER THE BENEFITS PROVISIONS, THIS PROGRAM DOES NOT COVER ANY LOSS CAUSED BY OR RESULTING FROM ANY OF THE FOLLOWING:
1. Routine physical examinations required for obtaining or continuing employment, requirement in school, insurance/travel or government licensing, health permit and other similar purposes.
2. Custodial, Domiciliary, Convalescent and Intermediate care
3. Professional fees of medico-legal officer/s
4. All expenses incurred in the process of organ donation and transplantation if the Member is the donor, and its complications.
5. Benefits covered by Phil health and all other government funded healthcare entitlements as provided for by law.
6. Purchase or lease of any Durable Medical Equipment, oxygen dispensing equipment, and oxygen except during covered in-patient care.
7. All pregnancy related conditions requiring medical and surgical care.
8. Circumcision (except treatment of urological conditions), sterilization of either sex or reversal of such, artificial insemination, sex transformation or diagnosis and treatment of infertility.
9. Cosmetic procedure and surgery and oral surgery solely for purpose of beautification, including but not limited to wart removals through excision or electrodessication/ cauterization except reconstructive surgery to treat functional defects due to disease or accidental injury.
10. Weight reduction programs, surgical operation or procedure for treatment of obesity, including but not limited to gastric stapling.
11. Dental care following accidental injury to teeth requiring reconstructive surgery, orthodontic procedures or supply of dentures.
12. Long term rehabilitation and all forms of behavioral disorders whether congenital or acquired; developmental or psychiatric disorder; psychosomatic illness.
13. Any injury, illness or condition which the Member may suffer after he has taken intoxicating drugs or alcoholic beverage as evidenced by clinical history or alcoholic breath as determined by the examining physician and/or conditions or illnesses resulting from Alcoholism and Drug Addiction.
14. Medical or surgical procedures that are experimental in nature and not generally accepted as standard medical treatment by the medical profession that may include but is not limited to, Chiropractic Services and Acupuncture.
15. Allergens used for hypersensitivity testing regardless if administered as an out-patient or in-patient procedure.
16. Injuries or illnesses resulting from hazardous activities in which a Member has engaged in leisure that may include but is not limited to: bungee jumping, scuba diving, hang-gliding, mountain climbing and all such other voluntary activities which pose a danger to life and limb, except those related to or directly connected with the Member’s occupation as declared in the application for health care coverage under the Agreement.
17. Injuries or illnesses due to military service or suffered under conditions of war.
18. Executive check-ups and confinement which are for purely diagnostic purposes except as specified in the Agreement.
19. Injuries or illnesses which are self-inflicted, caused by attempt at suicide, or incurred as a result of or while participating in the commission of a crime or acts involving the violation of laws or ordinances.
20. Take-home medicine, immunizing agents and out-patient medicines, with the exception of intravenous chemotherapy medicine and those administered during an emergency treatment.
21. Vaccines, whether elective or administered during an emergency treatment are not covered, except passive and active vaccine for anti-tetanus, anti-venom, and anti-rabies vaccine as specified in the Agreement.
22. Laser Treatment for the purpose of corrective eye refraction.
23. Medico-Legal Fees. These are professional fees of a medico-legal consultant to whom a patient is referred primarily for the issuance of a medical certificate for legal purposes.
24. Sexually transmitted diseases, AIDS and AIDS related diseases.
25. Congenital deformities and abnormalities unless specified in this Agreement.
26. Infectious diseases (according to the local epidemiological patterns) that may arise in times of an epidemic (i.e. Avian Flu, Meningococcemia, etc.) as declared by World Health Organization (WHO) and/or by Department of Health (DOH).
27. Dietary consultations, weight reduction programs, surgical operation or procedure for weight reduction, treatment of obesity, including gastric stapling or balloon procedures and liposuction.
| ACETONE/ALCOHOL |
| AMBULANCE FEE |
| ARM BAND/ ID BAND |
| BEDPAN |
| CALIBRATED GLASS |
| COLD/ HOT WATER BAG |
| DIAPER |
| DIET PLAN / DIETARY / DIETARY SERVICES |
| DISTILLED WATER / DRINKING WATER / MINERAL WATER |
| DRY SHEET / CURITY PAD |
| ELECTRICITY USED / RENT OF APPLIANCES (TV/REMOTE CONTROL/ELECTRIC FAN, ETC) |
| ENVIRONMENTAL LEVY/WASTE DISPOSAL FEE/PATHOLOGICAL WASTE |
| EXTRA BED / BEDDINGS (REGULAR) LAUNDRY / LINEN |
| EXTRA MEALS / SPOON & FORK |
| EXTRA PILLOWS / PILLOWS / PILLOW (SUITE ROOM) |
| FACE TOWEL / TOWEL |
| FAMILY PLANNING |
| HOSPITAL SERVICE FEE (UNSPECIFIED) |
| IV TRAY |
| KIDNEY BASIN |
| MEASURING CUP |
| MEDICAL CERTIFICATE / MEDICAL RECORDS |
| NAME TAG/WRIST BAND |
| OFFICE FORMS / PHOTOCOPY / FORMS/PHIC / CLAIMS PROCESSING / FAX |
| PRIVATE NURSE |
| RAZOR |
| SANITARY NAPKINS |
| SLIPPERS |
| SPECIMEN CUP |
| TELEPHONE BILLS / TELEPHONE CALLS / COMMUNICATION FEE |
| THERMOMETER |
| TISSUE |
| TONGUE DEPRESSOR |
| TRANSFER FEE |
| TUMBLERS |
| UNDERPADS |
| URINAL BAG / WEE BAG |
| VITAMINS / FOOD SUPPLEMENT / TAKE HOME MEDICINES |
| UNSPECIFIED MISC. |
| BLOOD TYPING |
| SCREENING TESTS |
| SHOE COVER |
| PPE |
| N95 / KN95 |
| ISOLATION GOWN/BLUE GOWN |
| HUMIDIFIER |
| HEAD CAP |
| JANITORIAL SERVICE / HOUSEKEEPING |
| CLINICAL SERVICES (NURSING, MEDICAL TECHNOLOGIST, RADIOLOGY TECHNOLOGIST, ORDERLIE) |
| SECURITY SERVICES |
| MAINTENANCE FEE (ELECTRICAL/MECHANICAL) |
| ORAHEX / MOUTHWASH / BATH KIT |
| DISINFECTION / SANITATION FEE |
| PREGNANCY TEST |
ELITE DENTAL
88367181
0917-315-4926
0925-521-5766
0917-507-9123
(02) 8556-2286
gian_capuyan@elitegroup.com.ph
1WWH
09178848859
09228986481
(02) 7592402
Advanced Telemedicine Access Inc. (ATACCESS) is enhancing the way you receive healthcare through our telehealth solutions made possible by the company’s committed workforce who are ever ready to adapt to the restrictive routine of the new normal.
Click here for the video tutorial.
AMAPHIL TEXT ALERT
AMAPHIL TRANSACTION HISTORY AND BENEFIT REVIEW
REQUEST LOA FOR OUTPATIENT CONSULTATION
REQUEST LOA FOR OUTPATIENT LABORATORY
HOW TO REQUEST LOA
HOW TO GENERATE A LOA DOCUMENT
AMAPHIL REIMBURSEMENT
AMAPHIL CUSTOMER SERVICE
AMAPHIL ACCREDITED DOCTORS
ATACCESS
OUTPATIENT BASIC CONSULTATION and OUTPATIENT-REFERRAL-TO-SPECIALIST:
- NAME OF CALLER
- PROVIDER’S NAME
- TYPE OF AVAILMENT
- COMPLETE NAME OF THE PATIENT / CARD NUMBER OF THE PATIENT
- COMPANY NAME
- VALID ID PRESENTED (IF AMAPHIL CARD PRESENTED ONLY ASK FOR DOB)
- CHIEF COMPLAINT
- NAME OF THE CONSULTING DOCTOR / SPECIALIZATION
OUTPATIENT CLINIC-SETTING and OUTPATIENT-LABORATORY:
- NAME OF CALLER
- PROVIDER’S NAME
- TYPE OF AVAILMENT
- COMPLETE NAME OF THE PATIENT / CARD NUMBER OF THE PATIENT
- COMPANY NAME
- VALID ID PRESENTED (IF AMAPHIL CARD PRESENTED ONLY ASK FOR DOB)
- GIVEN DIAGNOSIS
- PROCEDURES (IF WITH INNER LIMIT OR SMALL AMOUNT OF OP LIMIT ASK FOR THE EXACT AMOUNT OF THE PROCEDURES)
EMERGENCY:
- NAME OF CALLER
- PROVIDER’S NAME
- TYPE OF AVAILMENT
- NOTE: MUST BE FINAL CHARGES, IF NOT GIVE AN INITIAL LIMIT ONLY (NO LOA YET)
- COMPLETE NAME OF THE PATIENT / CARD NUMBER OF THE PATIENT
- COMPANY NAME
- VALID ID PRESENTED (IF AMAPHIL CARD PRESENTED ONLY ASK FOR DOB)
- CHIEF COMPLAINT
- GIVEN DIAGNOSIS
- PROCEDURES (IF WITH INNER LIMIT OR SMALL AMOUNT OF OP LIMIT ASK FOR THE EXACT AMOUNT OF THE PROCEDURES)
OUT-PATIENT SURGERY (OPD-OR):
- NAME OF CALLER
- PROVIDER’S NAME
- TYPE OF AVAILMENT
- COMPLETE NAME OF THE PATIENT / CARD NUMBER OF THE PATIENT
- COMPANY NAME
- VALID ID PRESENTED (IF AMAPHIL CARD PRESENTED ONLY ASK FOR DOB)
- GIVEN DIAGNOSIS
- PROCEDURE AND RVS CODE (ESTIMATE AMOUNT NET OF PHIC)
- SURGEON’S NAME (ASK IF ACCEPTING)
- ANESTH’S NAME (ASK IF ACCEPTING) (IF APPLICABLE)
IN-PATIENT ADMISSION:
ER LEADING TO CONFINEMENT:
- NAME OF CALLER
- PROVIDER’S NAME
- TYPE OF AVAILMENT
- COMPLETE NAME OF THE PATIENT / CARD NUMBER OF THE PATIENT
- COMPANY NAME
- VALID ID PRESENTED (IF AMAPHIL CARD PRESENTED ONLY ASK FOR DOB)
- CONTACT NUMBER OF THE PATIENT/GUARDIAN
- ASK IF ER LEADING TO CONFINEMENT/DIRECT ADMISSION
- CHIEF COMPLAINT
- ADMITTING DIAGNOSIS
- ATTENDING PHYSICIAN/SPECIALIZATION (ASK IF ACCEPTING AMAPHIL)
- ASK IF THERE ARE OTHER PHYSICIANS
- ROOM AVAILED
- IF CASE IS ACCIDENT ASK FOR IR/POLICE REPORT
DIRECT/ELECTIVE ADMISSION:
- NAME OF CALLER
- PROVIDER’S NAME
- TYPE OF AVAILMENT
- COMPLETE NAME OF THE PATIENT / CARD NUMBER OF THE PATIENT
- COMPANY NAME
- VALID ID PRESENTED (IF AMAPHIL CARD PRESENTED ONLY ASK FOR DOB)
- CONTACT NUMBER OF THE PATIENT/GUARDIAN
- ASK IF ER LEADING TO CONFINEMENT/DIRECT ADMISSION
- ADMITTING DIAGNOSIS
- PROCEDURE/SURGERY TO BE DONE
- SURGEON'S NAME (ASK IF ACCEPTING AMAPHIL)
- ANESTHESIOLOGIST (ASK IF ACCEPTING AMAPHIL)
- ASK IF THERE ARE OTHER PHYSICIANS
- ROOM AVAILED
- IF CASE IS ACCIDENT ASK FOR IR/POLICE REPORT
OUTPATIENT CLINIC-SETTING, OUTPATIENT-LABORATORY and OUT-PATIENT SURGERY (OPD-OR)
- CHECK DETAILS OF THE MEMBER (Name of requesting member should be the same name written in the doctor's request)
- CHECK ATTACHMENT
- ATTACHMENT SHOULD BE A DOCTOR'S REQUEST (DATE REQUESTED/DX/PROCEDURES/PHYSICIAN SIGNATURE)
INITIAL LIMIT OF THE MEMBER (50% of patient ABL/MBL except FL)
ROOM ENTITLEMENT (RBE & INCREMENTAL IF APPLICABLE)
REQUIREMENTS (REQUIRED TO FILE PHIC/CORP SPECIAL INSTRUCTIONS)
UNCOVERED ITEMS (BRIEF ONLY): MISCELLANEOUS FEEs & PERSONAL ITEMS LIKE PILLOWS, LINENS, FOODS/SNACKS, VITAMINS, TAKE HOME MEDICINES
ASK THE PROVIDER IF THEY HAVE OTHER QUESTIONS ASIDE FROM WHAT WAS DISCUSSED
INFORM THEM THAT IF THEY HAVE FURTHER INQUIRIES/QUESTIONS JUST CALL US IN OUR HOTLINE OR MAY EMAIL US AT mo@amaphil.com.ph
MAXIMUM LIMIT (Explain to the member regarding the initial limit relayed to the provider)
ROOM ENTITLEMENT (RBE & INCREMENTAL IF APPLICABLE)
REQUIREMENTS (REQUIRED TO FILE PHIC/CORP SPECIAL INSTRUCTIONS)
UNCOVERED ITEMS (BRIEF ONLY): MISCELLANEOUS FEEs & PERSONAL ITEMS LIKE PILLOWS, LINENS, FOODS/SNACKS, VITAMINS, TAKE HOME MEDICINES
Please note that the below processes are assuming that the availment is covered, checking of SOB and utilization is not included:
OUTPATIENT BASIC CONSULTATION and OUTPATIENT-REFERRAL-TO-SPECIALIST
OUTPATIENT-LABORATORY
OUTPATIENT CLINIC-SETTING
OUTPATIENT FACILITY FEE
EMERGENCY
OUT-PATIENT SURGERY (OPD-OR)
INPATIENT ADMISSION
Requirements: SOA, itemized charges, OR-Tech (if applicable) and additional documents are requested as needed (medical abstract, certificate of room-nonavailability, etc.)
Coverage will be based on the FINAL DIAGNOSIS
Turn-around-time of processing is 15-30mins only
Check the members coverage based on the final diagnosis:
- PEC?
- Exclusion?
- Inner limit?
Check the members utilization:
- Remaining limit?
Check the RNB entitlement:
- If within the member's RNB entitlement. proceed
- If not, compute for RBE and incremental (if applicable)
Check for the uncovered items:
- Get each uncovered items with their corresponding amount
Check the physicians:
- For medical management:
- Is the physician accepting amaphil?
- Number of visit days? (If only 1 physician is reflected in the SOA, process PF from admission to discharge; If multiple physicians, verify the number of visit of each physician to the provider)
- If room availed is not within the patient's room entitlement, compute PF excess.
- For surgical management:
- What is the surgery done? RVS code/s?
- Is the physician accepting amaphil?
- What is the procedure done by each physician listed in the SOA? (verify this to the hospital if not indicated in email)
- If room availed is not within the patient's room entitlement, compute PF excess.
Finalize total amount c/o patient and/or other remarks, then proceed encoding in allaccess.
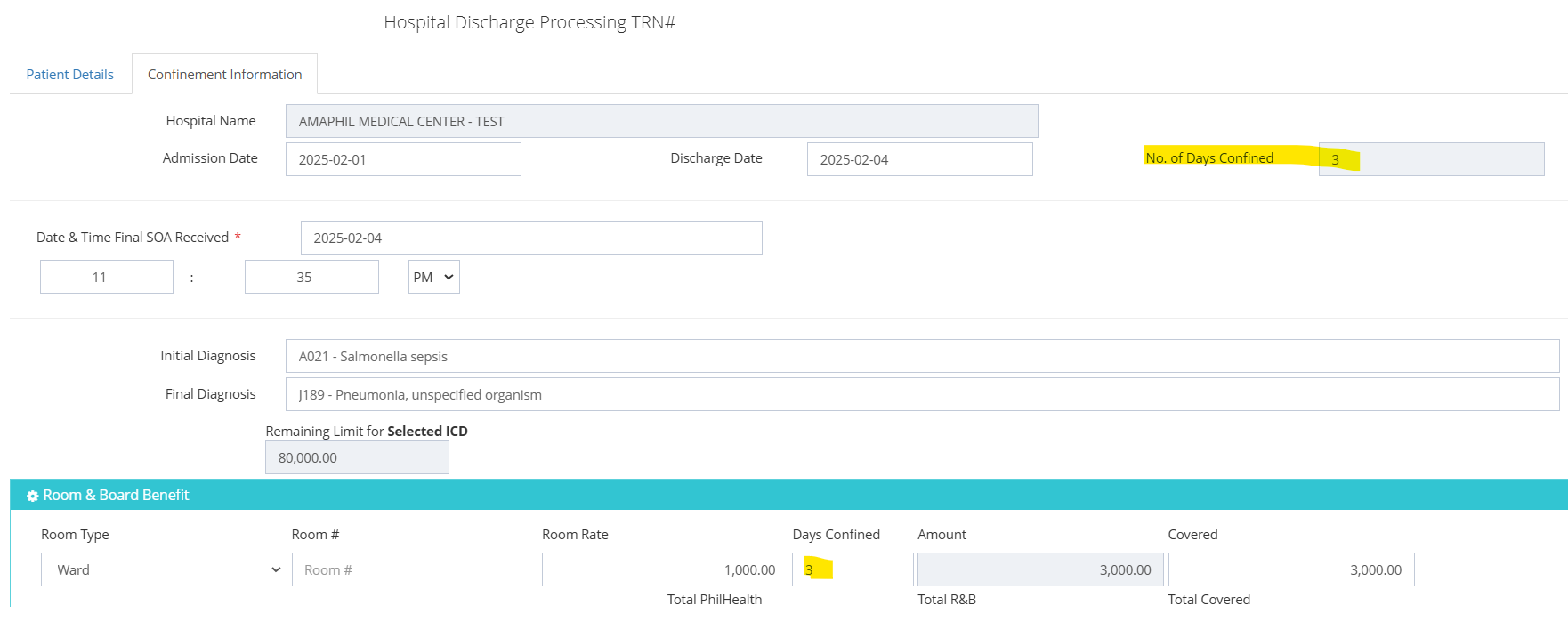
ENCODING IN ALL ACCESS:
- Double check admission/discharge date based on the SOA received, edit dates if needed.
- Date and time received of SOA/itemized charges will be based on email.
- Encode the ICD code of the FINAL DIAGNOSIS.
- Encode room and board:
- Room category - encode the category based on the room availed by the patient.
- Room amount - encode based on the room entitlement of the patient
- Days confined - encode based on the reflected number of days confined in allaccess:
- Encode RVS code (if applicable)
- Encode in particulars portion: SUPPLIES and UNCOVERED ITEMS only.
- Encode in the "uncovered items" portion the the total HB amount c/o patient first.
- To get the amount to be encoded in the "supplies" portion: Gross HB less discounts (if applicable) less covered amount in room encoded less encoded amount in "uncovered items" portion.
- Encode PHIC amount (HB only).
- Encode payable physicians. (If no payable physician encode period (.) or dash (-) in "physician" portion, put attending physician, then zero (0) amount.
- Click "finalize computation" button.
- If with Corporate Guarantee (CG),
- Check mark the "Corporate Guarantee" button.
- Attach the CG letter or screenshot of the email endorsement of CG.
- Check if encoded amount in allaccess is tally with the SOA: TOTAL COVERED + TOTAL EXCESS - TOTAL PF = SHOULD BE TALLY IN THE NET HB IN SOA
- Encode the uncovered items remarks or any remarks necessary.
- Upload necessary documents (SOA, itemized, or-tech, etc.)
- Click "discharge" button.
- To download the LOA, go to the "transaction generator" search the TRN.




